How to review assessments
In this guide, you will learn about:
- How to open an assessment
- Multiple assessment forms and statuses
- How to edit an existing form or send a new form to the patient
- Clinical notes and suggested tasks
How to open an assessment
To open an assessment, head to the Assessment tab on the patient page. You will be able to view the assessment on the right hand side.
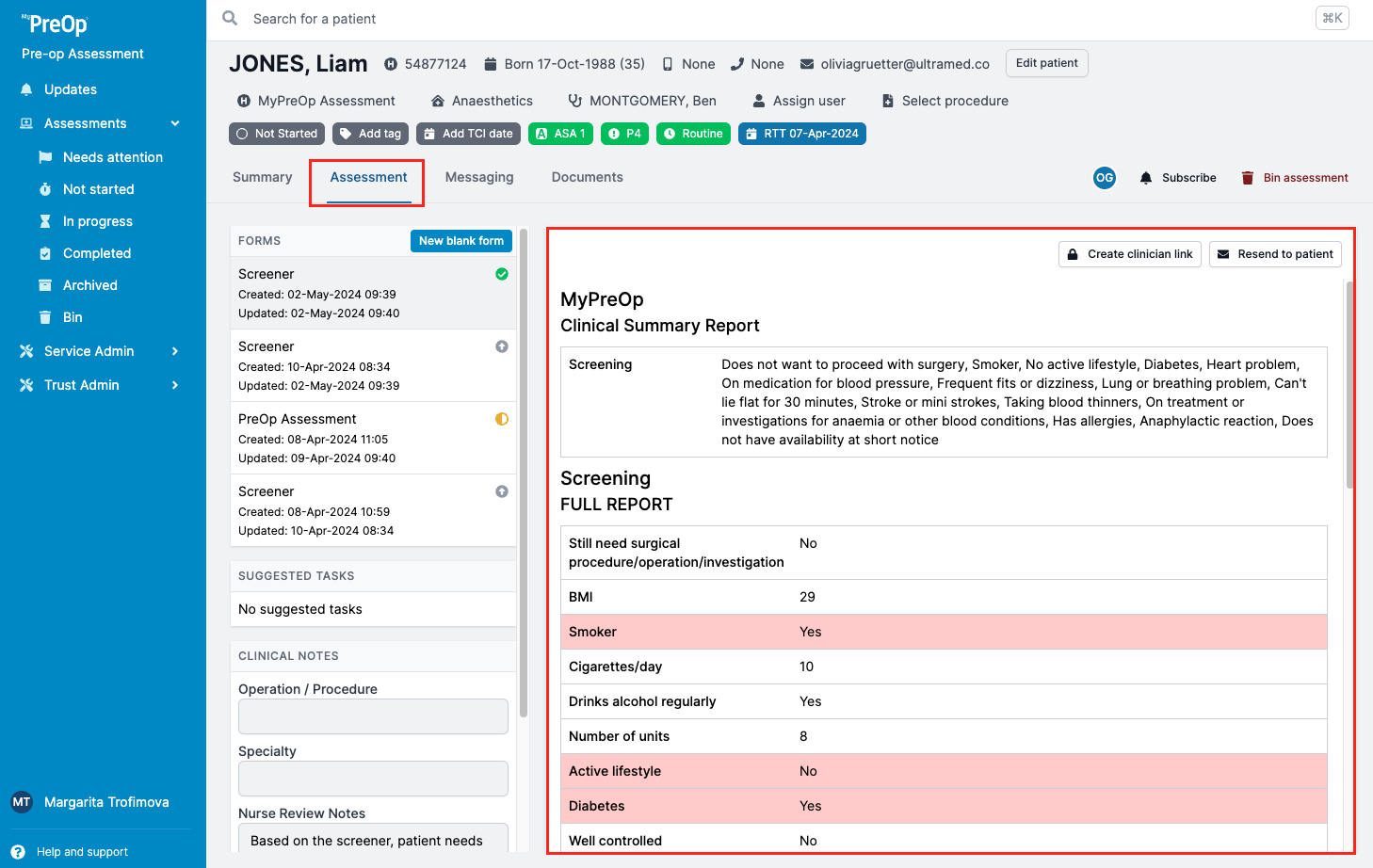
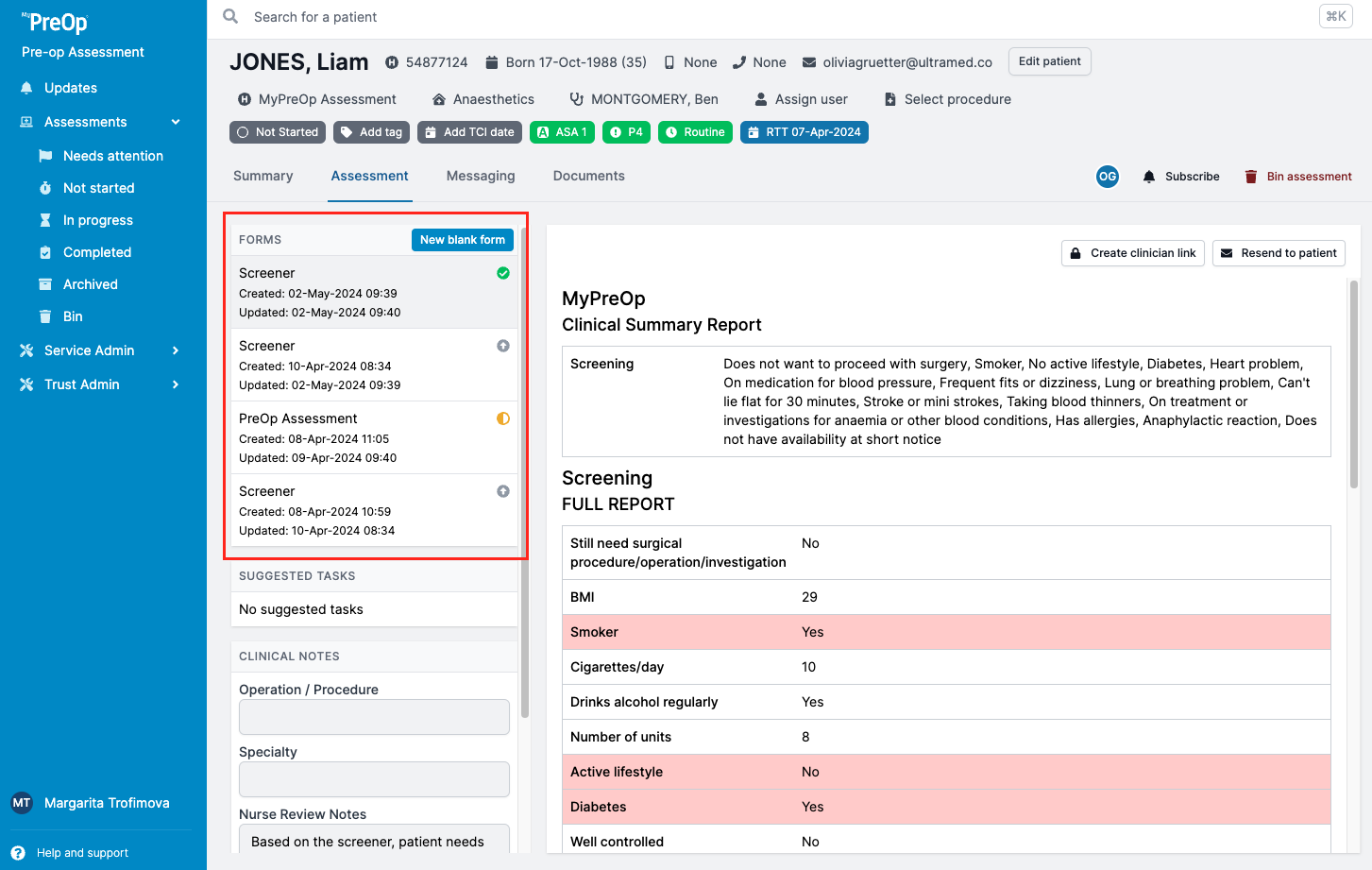
Multiple assessment forms and statuses
You will be able to see all available versions of the assessments, as well as its status on the left in the Assessment tab.
To learn about the status of the assessment, view its progress and see the patient answers as they are added, simply click on the form from the list. The amber banner at the top of the assessment will show all information related to the assessment.
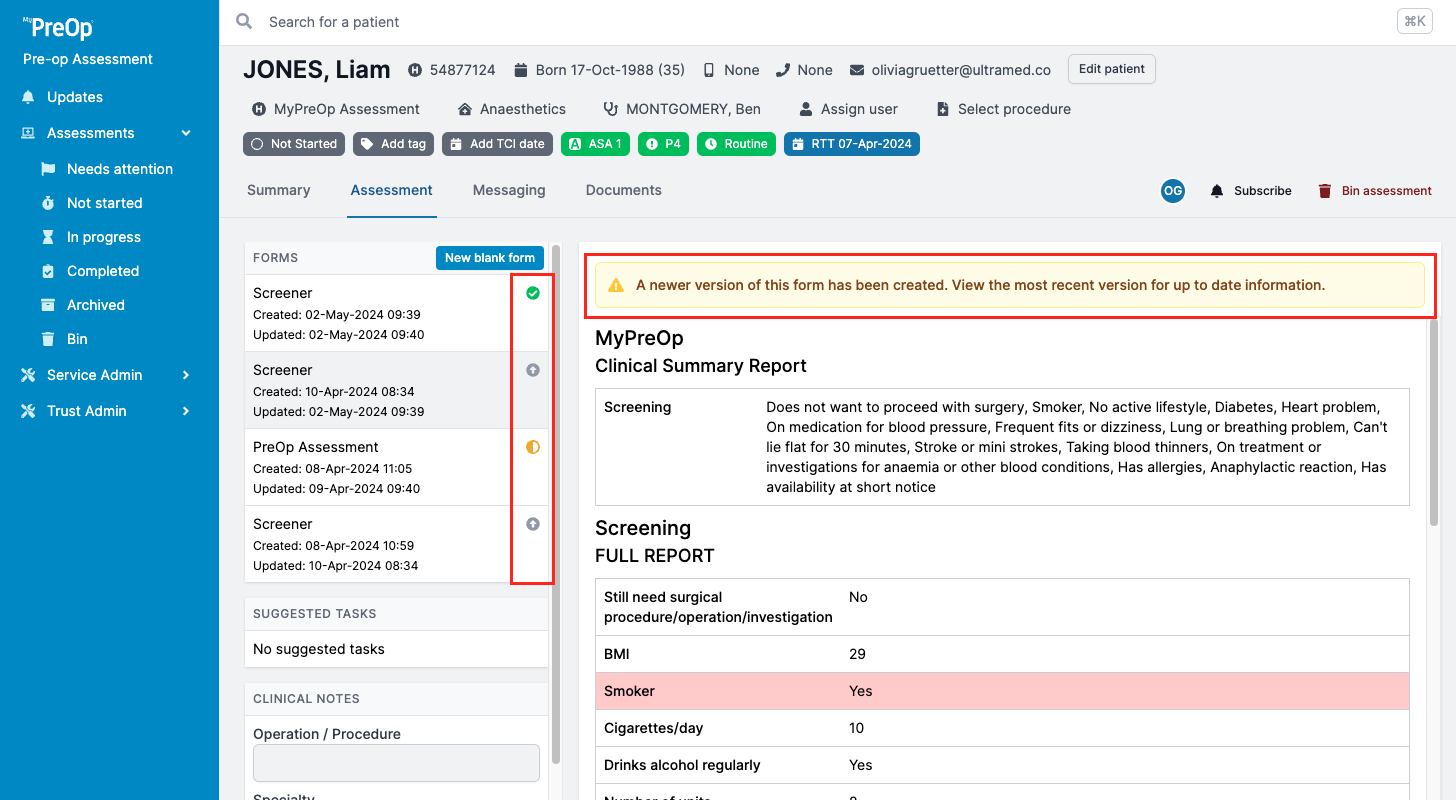
Moreover, you can view the status of the assessment by checking the icons on the right of the form list:
- Green - assessment submitted
- Amber - the form is empty or in progress
- Grey - a newer version of the form is available
- Red - invite failed to send
- Clear - invite has not been sent
How to edit an existing form or send a new form to the patient
To make changes to the existing form, use the buttons above the assessment.
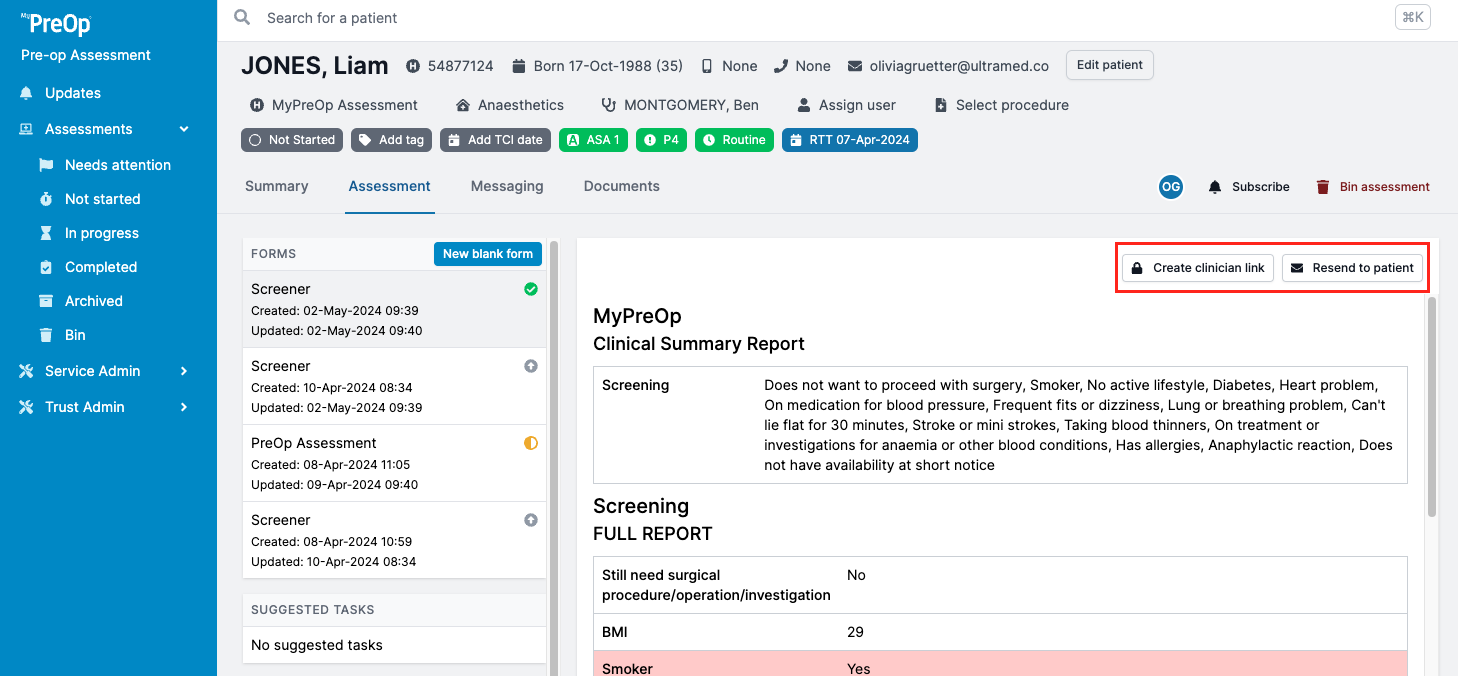
“Create clinician link” will allow you to access a patient's existing assessment and make changes or add to their answers.
“Resend to patient” will resend a new invite to the patient, which will allow them to review and update existing assessment.
“Cancel” button will allow you to cancel a patient's invite and prevent them from accessing the assessment. It will also reactivate the previous version of the same form.
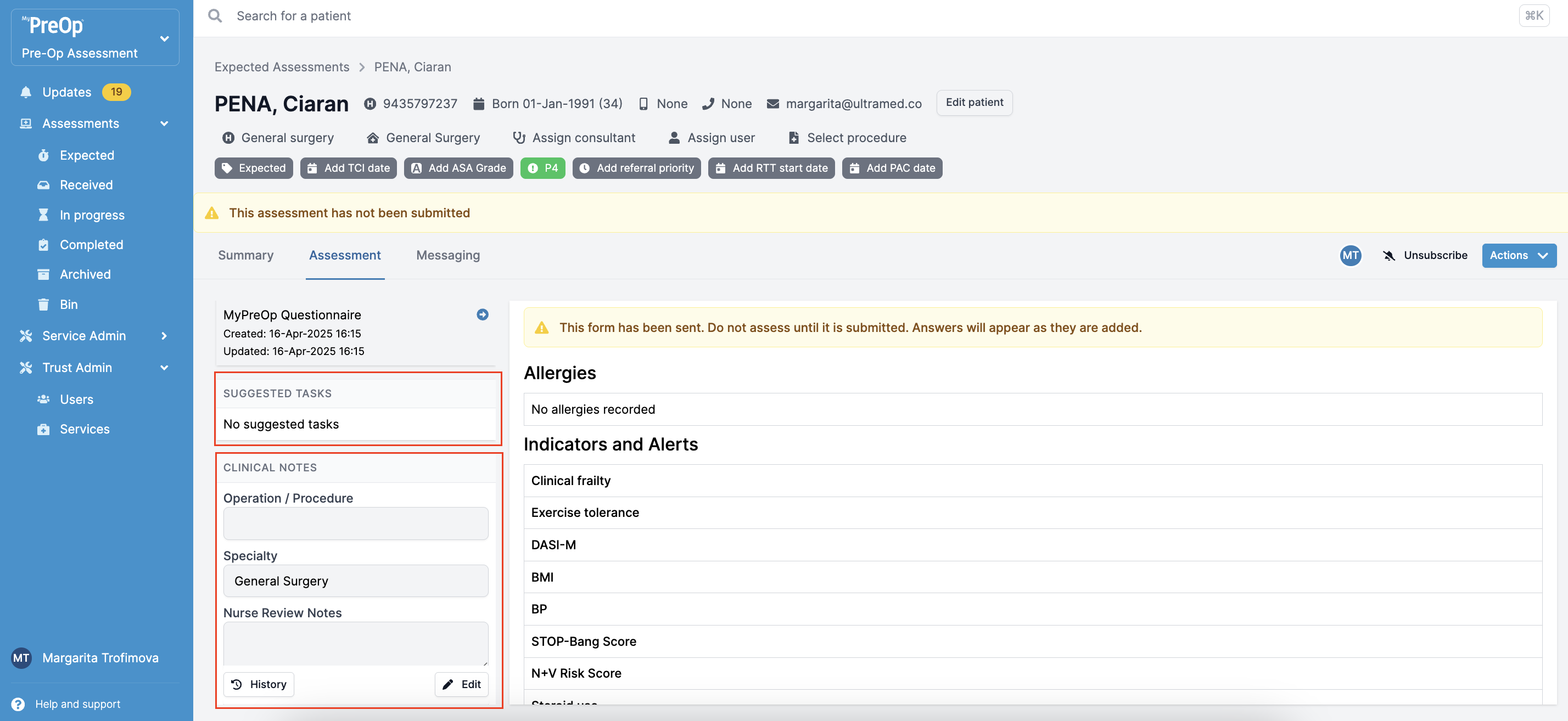
Clinical notes and Suggested tasks
On the left hand side of the Assessment tab, you will see the Suggested Tasks. You can click on each task and make any necessary changes and add notes. Remember to click ‘Save’ when done.
Scrolling down in the left-hand tab, you will also find the Clinical Notes. To make changes, click the ‘Edit’ button and click ‘Save’ when complete.
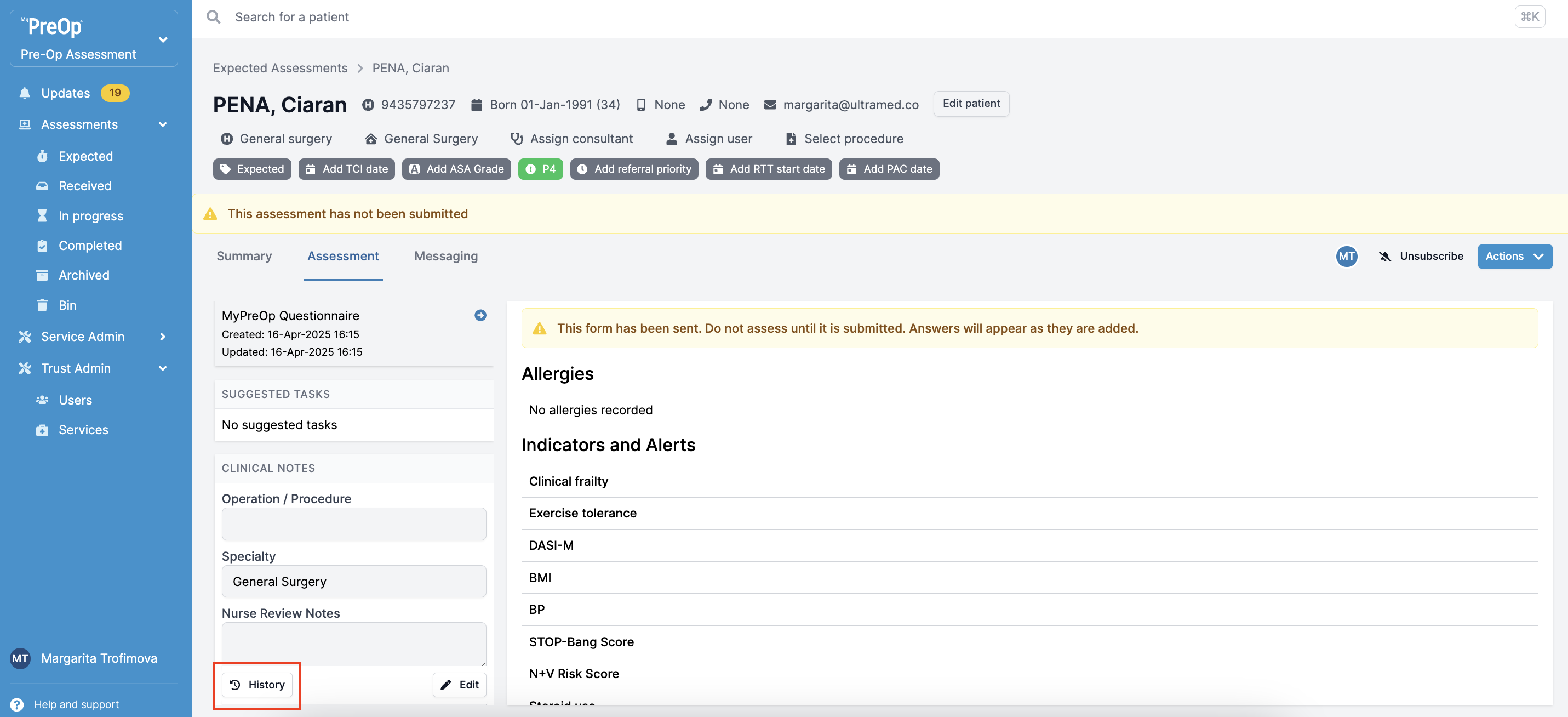
Clinical Noting History
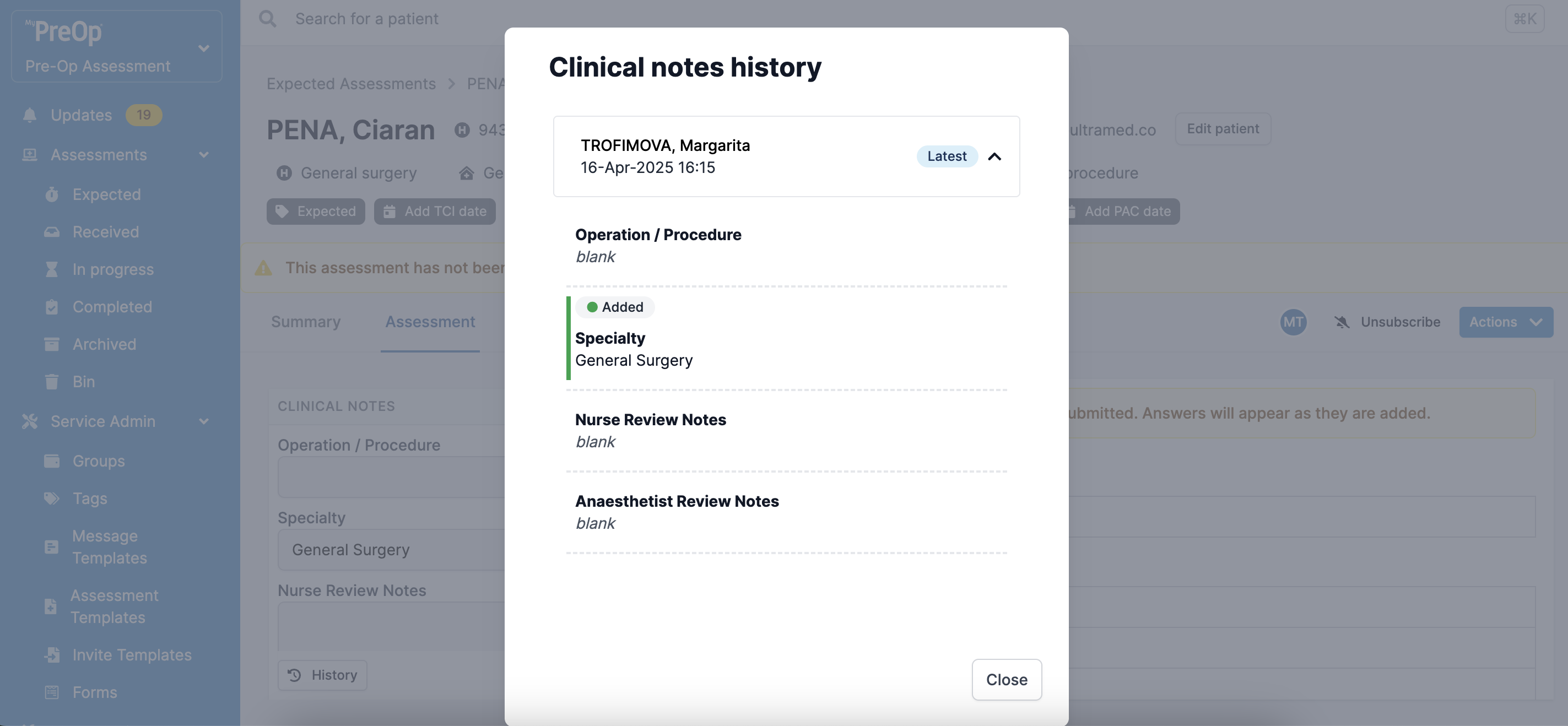
"History" button in the bottom left corner allow the users to view the history of the clinical notes, as well as trace their authors.
Once you click on the "History" button, a pop up will appear, showing the timeline of the updates. You can expand each update to view the changes.
Please note that these changes are only available for the assessments created after 10th of February 2025.
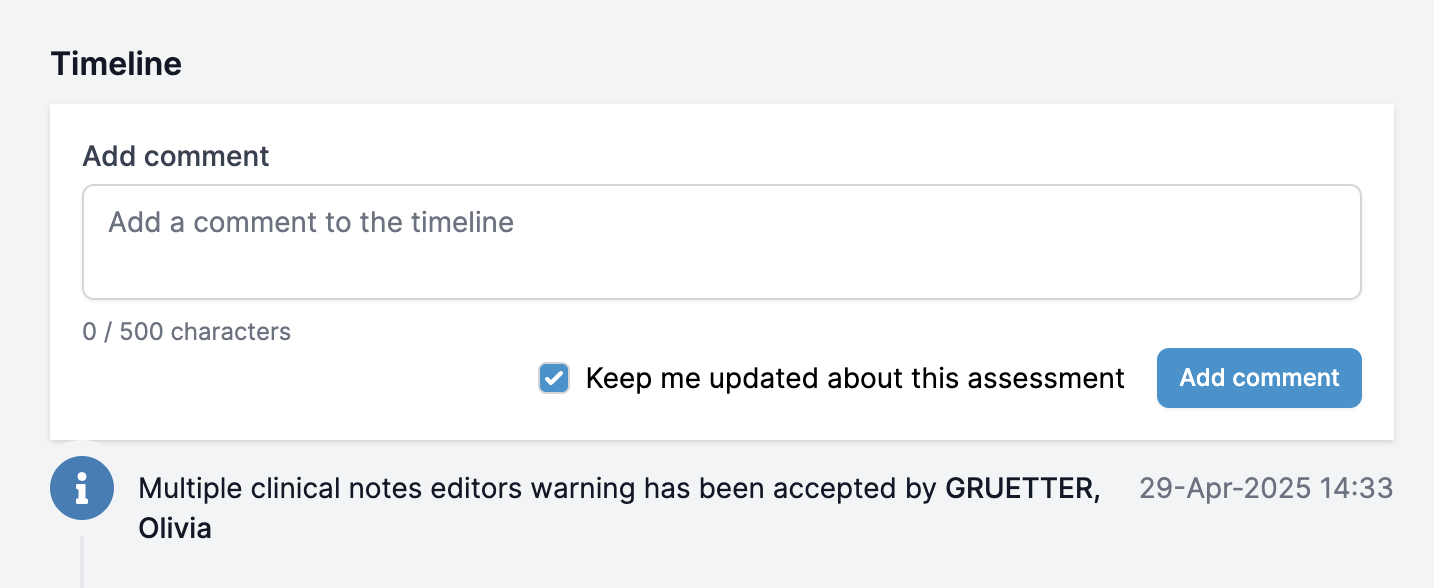
Multiple Clinical Notes Editors Warning
The system will also warn you about saving the changes, in case multiple users are editing the same clinical noting section:
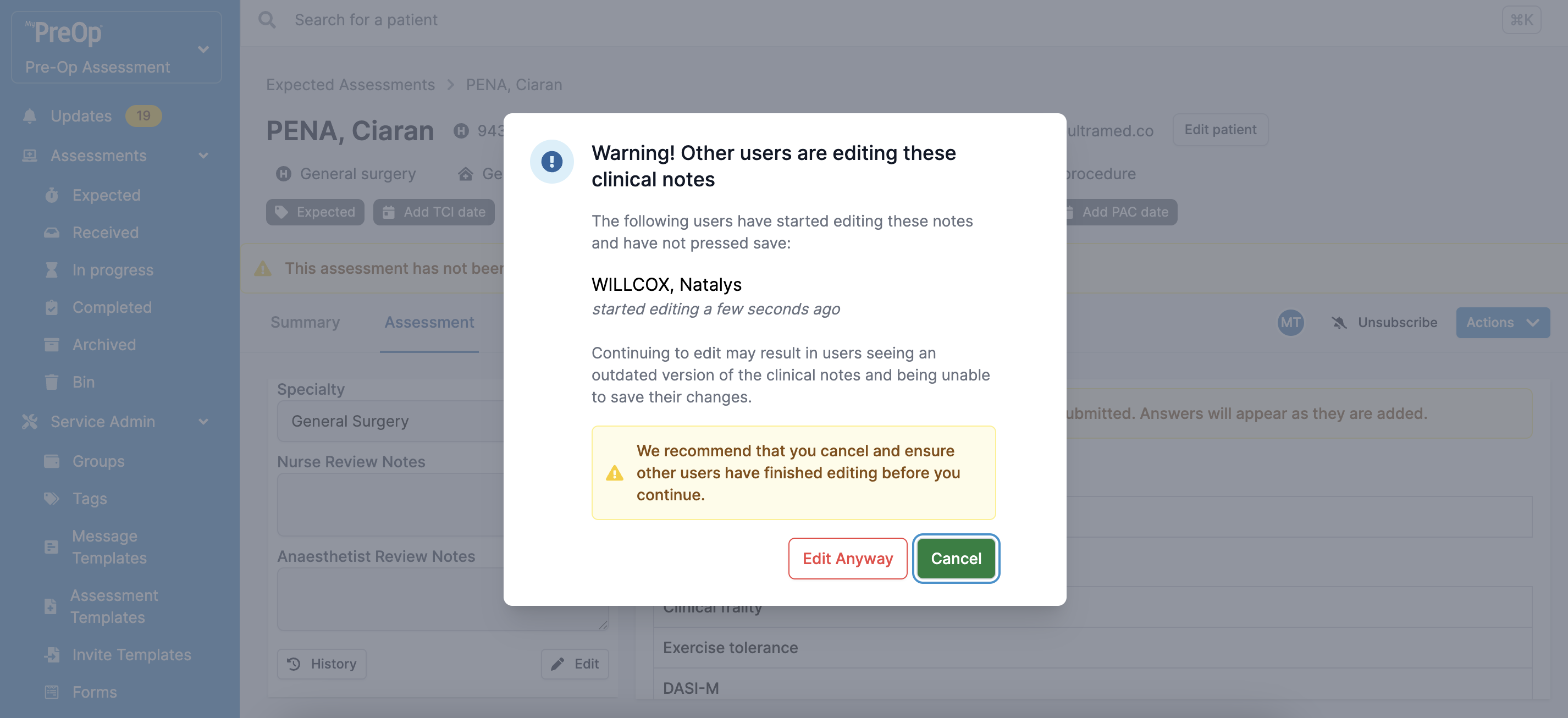
You can choose to continue editing or cancel your changes. In this case, the Timeline will record your decision:
It is important to note that continuing to edit may result in users seeing an outdated version of the clinical notes and being unable to save their changes.
Please note that due to individual portal configurations, some features might look different in your live portal.